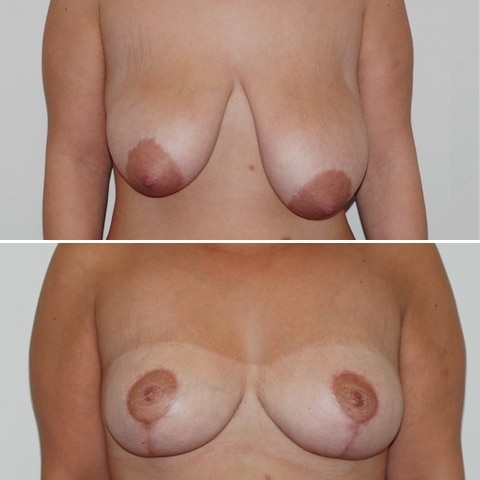
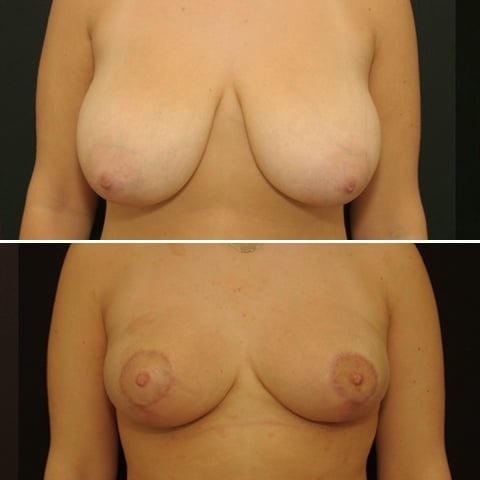
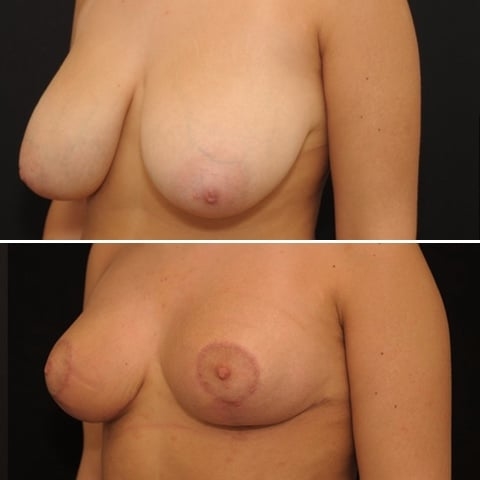
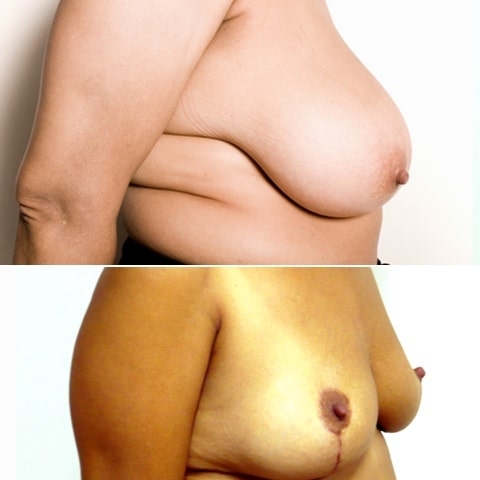
Réduction mammaire
Les points forts
- Réduction du volume et de la ptose mammaire
- Intervention prise en charge par la sécurité sociale sous conditions ( ablation de 300 g par sein opéré)
- Grande satisfaction des patientes
Description
La réduction mammaire a pour but de réduire le volume de la glande mammaire et de modifier la forme et la position du sein.
L’intervention consiste en une réduction du volume mammaire, en retirant la glande située à la portion inférieure du sein.
La glande restante est ensuite remodelée et remontée vers la portion supérieure du sein.
L’aréole et le mamelon sont ainsi repositionnés vers une position idéale située au sommet du sein.
- verticales dans de rares cas (patiente jeune et hypertrophie modérée)
- le plus souvent verticales et horizontales: technique dite en « T » ou en ancre marine qui sont effectuées la plupart du temps
Intervention
Si vous avez des antécédents familiaux de cancer du sein, une mammographie et une échographie peuvent vous être demandées.
La réduction mammaire est réalisée sous anesthésie générale. Ceci nécessite une consultation pré-anesthésique au minimum 48 h avant l’intervention.
Dans la majorité des cas, l’intervention est réalisée en hospitalisation conventionnelle (entrée à 13h sortie à 11 h le lendemain) mais peu parfaitement s’envisager en chirurgie ambulatoire (entrée à 8h, sortie à 18h) .
L’opération est peu douloureuse mais les soins post-opératoires nécessitent d’arrêter son activité professionnelle pendant 5 à 7 jours.
Nos Spécificités
Contrairement à la majorité de nos confrères français qui utilisent une technique à pédicule supérieur, nous utilisons une technique opératoire spécifique (technique du pédicule supéro-interne) décrite par une chirurgienne canadienne (Elisabeth Hall-Findlay).
Cette technique à l’immense avantage de ne pas séparer l’aréole et le mamelon de la glande sous jacente. Ceci permet :
- d’éviter quasiment tout risque de nécrose de l’aréole et du mamelon (5% des cas avec la technique à pédicule supérieur)
- d’améliorer fortement la sensibilité post opératoire de l’aréole et du mamelon et préserver cette zone érogène
- de pouvoir envisager un allaitement après une réduction mammaire (impossible avec la technique à pédicule supérieure.
Cette technique permet aussi de limiter les décollements de tissus importants et permettre une chirurgie de réduction mammaire en ambulatoire sans pose de drain de Redon
Questions / Réponses
Quelles sont les complications possibles d’une réduction mammaire ?
La complication principale est l’altération de la sensibilité de l’aréole et du mamelon. Celle-ci survient dans environ 30% des cas et peut persister à long terme.
Un hématome ou caillot de sang peut survenir le soir de l’intervention mais ceci est extrêmement rare.
En cas de seins extremement volumineux, une souffrance de l’aréole peut survenir dans 5% des cas nécessitant une greffe de l’aréole pendant ou le lendemain de l’intervention.
Les cicatrices sont initialement épaisses et inflammatoires les 3 premiers mois, puis dimimuent fortement jusqu’à 18 mois après l’intervention.
Quels sont les soins post-opératoires ?
Les soins post-opératoires sont relativement simples.
Le lendemain de l’intervention, les drains vous sont retirés par l’infirmière et les soins sont effectués après la douche.
Ils consistent en une désinfection de la cicatrice suivi de la mise en place de pansements ou de compresses dans le soutien gorge de sport.
Ces soins sont répétés tous les jours à votre domicile pendant 15 jours, éventuellement aidée d’une infirmière les premiers jours.
Le soutien gorge de contention est à garder en permanence jusqu’à 3 semaines après l’intervention.
Quel va être mon bonnet après l’intervention ?
La majorité des patientes nécessitant une réduction mammaire ont un bonnet supérieur au E.
Afin de conserver un galbe du sein harmonieux, il est nécessaire de garder un volume mammaire équivalent à un bonnet C.
Certaines femmes souhaitent un bonnet B, mais elles doivent être prévenues que les seins risques d’être un peu plats et moins esthétiques.
Peut-on allaiter après l’intervention ?
C’est fortement déconseillé.
En effet, comme la chirurgie de réduction mammaire sépare l’aréole de la glande sous-jacente, les canaux galactophoriques amenant le lait sont coupés.
Il existe un risque très élevé (plus de 80%) d’engorgement mammaire lors de la montée de lait qui peut évoluer vers une infection.
Combien coute une réduction mammaire ?
L’assurance maladie prend en charge les réductions mammaires dont la pièce de résection glandulaire est supérieure à 300g par sein opéré.
Cela correspond en pratique à un gros bonnet D.
Dans ces cas, je pratique des compléments d’honoraires complémentaires qui varient entre 2000 et 3000 euros, pouvant éventuellement pris en charge par votre complémentaire santé.
Si la résection glandulaire prévue est inférieure à 300g, les prix correspondent à ceux d’une cure de ptôse simple (de 4500 à 5500 euros)
Une question ? Contactez-nous !
Le cabinet
Docteur Yaël Berdah et Docteur Marc-David Benjoar
Chirurgiens esthétiques à Paris France